1. Is PHN common?
Over half the 194,000 people with shingles each year (that’s the number for England and Wales) are affected by post herpetic neuralgia (PHN).
PHN is the name given to the shingles pain when it has been going on for a month or more after the shingles sores have healed.
Shingles is not something that other people will catch from you.
You can watch a video about postherpetic neuralgia here:
2. What is PHN like?
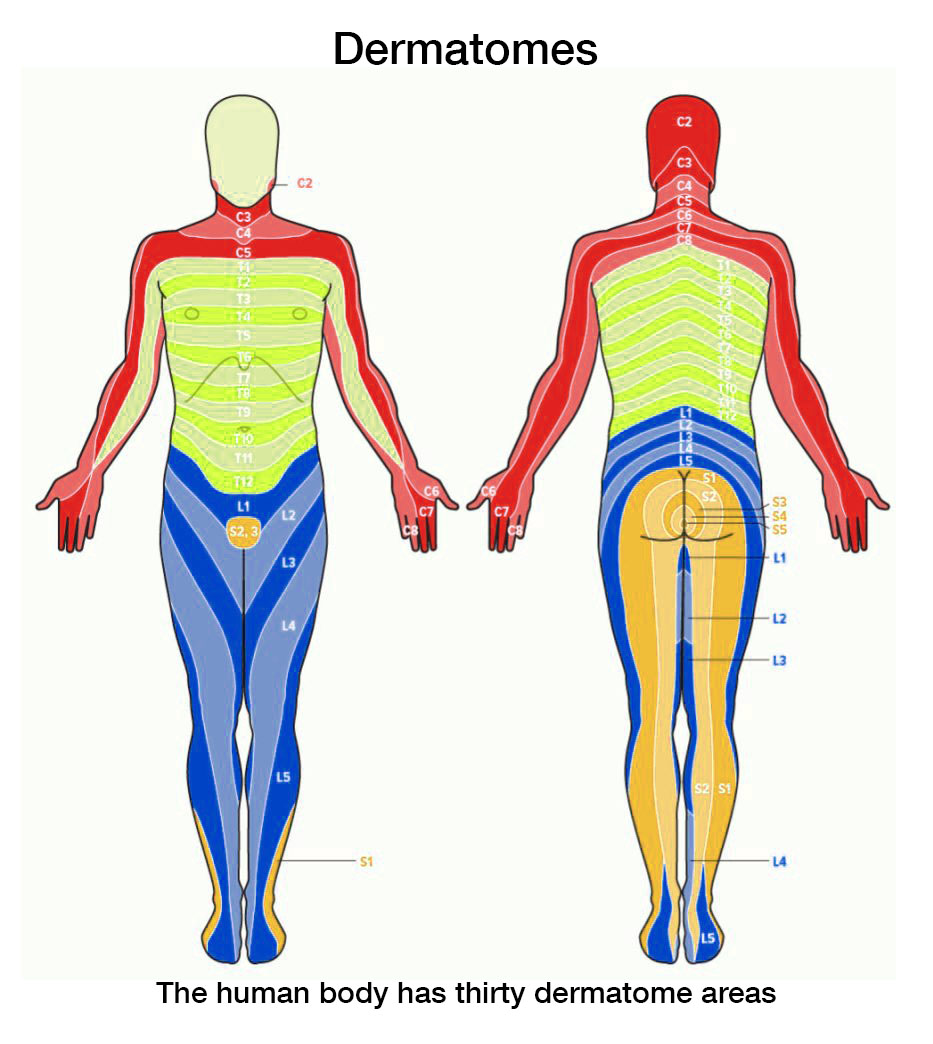
Post herpetic neuralgia can be felt as itching, irritation, stabbing, burning, tingling, supersensitivity, numbness or soreness but to simplify our text we will always call it “pain”. If this happens, it will be in the area where you had the shingles – not elsewhere on your body.
The chart shows the dermatomes, or ‘slices’ of body served by each nerve ganglion. Any of these ‘slices’ could have symptoms of shingles. And each rib (in the green area) is in its own dermatome.
3. When does PHN happen?
Post herpetic neuralgia may begin as the symptoms of shingles subside and can last a few weeks, months or occasionally years. It can appear several weeks or even months after the shingles has gone.
4. Why does PHN happen?
PHN happens when the chickenpox virus damages a sensory nerve during the shingles outbreak. The damaged nerve sends abnormal messages or even stops sending them so there is numbness. Sometimes there can be changes in nerves in the spinal cord – this is why cutting the affected nerve does not stop the pain of PHN.
As you get older, your chance of developing PHN increases.
5. How can PHN be treated?
It is difficult to treat this kind of pain. Your doctor can prescribe strong pain killers, but often these have little effect on post herpetic neuralgia. Other strong prescription painkillers (opioids) have helped some people, so they may be worth a try.
Pain killing drugs work almost immediately. But after a matter of hours, their effect will fade away. So you need to take them regularly, as prescribed.
However, there are other forms of medication that your doctor may prescribe. And these can be surprisingly effective. The important thing to know about these “pain blocking” treatments is that it will be weeks before you will notice an improvement. They slowly build up the pain block, day by day.
These treatments include pills, plasters/patches and creams – so don’t give up hope:
- Antidepressant drugs: If your doctor has prescribed one of the tricyclic drugs to combat PHN, you may find it causes drowsiness and/or a sensation of ‘dry mouth.’ The most commonly prescribed drug is amitriptyline. You should start off at a very low dose, probably 10 mg, and gradually build it up. ‘Dry mouth’ can be alleviated by sips of water or fruit juice, or by sucking a sweet or mint. (NB you can buy sugar-free or diabetic sweets if you are controlling your weight.) These side effects will wear off when you’re used to the treatment. As Mrs S. reported: “… it did ease the dreadful pain. I had one or two side effects when taking the pills but I could cope with them – to ease the pain was the main thing and amitriptyline did that.”
- Anti-epileptic drugs: Gabapentin (which was developed to control epilepsy) has been shown to be an effective way to block PHN and has been licensed by the Medicines Control Agency for treating PHN and other neuropathic pains. (In the US it is now used more for controlling pain than epilepsy!) Start with a low dose, probably 300 mg twice a day, and increase over the next weeks/months. It does not interfere with other medication you may be taking and has remarkably few side effects even with dosage as high as 800mg three times a day.
- Axsain cream (made from chilli peppers or ‘capsaicin’) has been discontinued. You may find it mentioned in shignles pain treatment advice but for some years now it is not obtainable in the UK.
- Versatis plasters are large ‘patches’ which can now be prescribed for PHN. These are made with a special gel allowing the active ingredient, lidocaine, to seep into your skin. You wear one for 12 hours (day or night as you prefer) on or near the painful area and leave the skin open to breathe for the other 12 hours. They are particularly helpful for people who don’t want to take pills.
- Chilli pepper patch – “Qutenza (capsaicin) 8%” is a new treatment that medical personnel at specialist pain centres around the country are being trained to use. It is a skin patch containing a synthetic equivalent of the naturally occurring capsaicin compound found in chilli peppers. A doctor or nurse will numb the area using an anaesthetic cream and the patch is then applied for one hour. This treatment should reduce or eliminate the pain of PHN for three months, after which the treatment can be repeated if it has helped.
You can see the details of treatment dosage on the guideline written by a pain specialist.
6. What can I do to help myself?
The Shingles Support Society’s 17-page information pack includes 2 pages of ‘Readers’ Tips’ – you can see some of them here. These are suggestions from others who are living with PHN. These are alternative ways of dealing with pain. These have not been proved scientifically, so we cannot endorse them but people have told us that they find them helpful. Send a small donation to the Shingles Support Society. Or you can buy it here.
7. Could a TENS machine help?
Transcutaneous electronic nerve stimulation (TENS) machines give tiny buzzing sensations and these prevent the nerves from sending their false pain messages to the brain. You should be able to try a TENS unit before you buy it to see if you are one of the people who benefits from it – or make sure the company has a money-back guarantee.
8. Can shingles be prevented?
There is a vaccine provided by GPs for people who are 70 to 79 years old on September 1st, 2020. It prevents half the cases of shingles and lessens the severity of the cases that do happen. We recommend, therefore, that you have this vaccine if you are in the age group.
From 1st September 2023, the new Shingrix, double dose vaccine, will be offered to people who become 65 years old. We have written about the new shingles vaccine here.
9. Can I contact others with the same problem?
The Shingles Support Society’s 17-page information pack includes a list of patients like you with post herpetic neuralgia who would like to hear from other people. Often communicating with someone else who knows what it feels like can be helpful and reassuring. Please let us know if you would like to be added to the list. Send an SAE with a small donation to the Shingles Support Society; or you can buy it here.
10. Could I be referred to a Pain Clinic?
Your doctor could refer you to a pain clinic: https://www.nhs.uk/Service-Search/other-services/Pain%20management/LocationSearch/1426 either NHS or private.
If you send your postcode to British Pain Society, Churchill House, 35 Red Lion Square, London WC1R 4SG ([email protected]), they will send details of your nearest clinic.
11. Where else might I find information about pain?
British Pain Society has more information on where you can get treatment and the kinds of pain that people can have.
12. Help the Shingles Support Society
The Shingles Support Society is a sub-group of the Herpes Viruses Association (HVA) a registered charity, offering support to patients. As a voluntary organisation, we depend on your donations to enable us to continue to serve the community – we rely on your generosity.
Please would you make a donation? Any amount will help, no matter how small. Cash or postage stamps, cheques or postal orders (made out to ‘SSS’) will help to ensure our work continues. Click here to find out how to donate. Or you can click through to the shop area here and go down the page to where you can order the full 19 page “Shingles Information Pack” as described above.
Perhaps you would consider making a legacy. Thank you!
Marian Nicholson, Director
13. Bequests
We know that many people leave money to charities in their wills. We would really appreciate it if you would consider this kind of donation. If you already have a will, you can leave something to the Shingles Support Society in a codicil, that is an addition to your existing will. This is easier (and cheaper) than getting a whole new will.
We were left money by Mr Stone, whose son informed us: “My father found the information that you supplied made such a difference to his quality of life in his final years that he wants others to benefit as well.”
Mrs Scott’s church arranged a special collection for us in her memory and donated it to our charity. We were very touched.
Mr Goldman asked the Rotary Club he was very involved with to send the money raised after his death to us. “The Shingles Support Society is my favourite charity” he told them.
As a registered charity (no. 291657) we submit details annually to the Charity Commission so that it can ensure that we are fulfilling our constitutional ‘statement of aims’. You can be sure that your legacy would go to help spread information about treatments for shingles and PHN to everyone who needs it.
This page was written under the Information Standard rules.
Issued on 29-3-19
Updated 4-7-2024 Review date: no later than 4-7-2027
Full references for the statements made can be sent on request. Send us an email at [email protected].
The Information Standard states: The HVA and SSS shall hold responsibility for the accuracy of the information they publish. Neither the Scheme Operator nor the Scheme Owner shall have any responsibility whatsoever for costs, losses or direct or indirect damages or costs arising from inaccuracy of information or omissions in information published on the website on behalf of the HVA and SSS. Disclaimer: note that the blog and other personal experience stories are excluded from the scope of IS certification.


